11 Sept 2022, By Shivash Bhagaloo
An Actuary’s Advice to Medical Insurers
An Actuary’s Advice to Medical Insurers
Shivash Bhagaloo is a Fellow of the Institute and Faculty of Actuaries and Consulting Actuary at Lux Actuaries & Consultants
Changes in GCC regulation over recent years have necessitated the Actuary playing a central role in reserving, pricing, solvency assessment and risk management. In meeting these changes, those insurers that are forced to reorganise considerably struggle the most as legacy systems, processes and (most notably) people anchor them in the past.
Since medical insurance constitutes the lion’s share of KSA and UAE GWP for 2016, the deficiencies in this line are more consequential. Yet over and above this, the best practice approaches that govern how successful health insurers operate have been slow to spread, partially due to the ‘firefighting’ that has arisen from overwhelming regulatory change. Added to this there is a lack of understanding of the finer details of how a medical insurance department should function.
This article provides best practice advice to health insurers following observations made by looking at the local and international market through the actuarial lens.
Reserving
Medical underwriters must necessarily buy in to the way that reserves, as booked by the insurer, are calculated by the Actuary. There is usually a disconnect between views on gross and net loss ratios due to a misunderstanding of actuarial methods. Triangulations of claims (i.e. claims delay patterns) must be demonstrated to underwriters and claims managers and sufficient discussion and debate should occur. The ‘number of days of IBNR’ rule of thumb approach usually applied should be avoided as the assumptions implicitly made within this simplification are hardly ever tested and, if tested, are usually invalid.
The method of calculating allocated and unallocated (i.e. overhead) expenses of the medical department must be understood clearly as performance targets are (or at least should be) linked to such metrics as expense ratios and combined ratios. It is currently common for medical departments to labour under false impressions of the expenses allocated to their departments and the subsequent profitability shown in actuarial reports.
Underwriters and claims managers should read the actuarial reserving reports and provide feedback on, for instance, loss year versus underwriting year differences. This strengthens the overall compliance function, increases buy-in and subsequently elevates the intelligence of conversations between the internal and external parties related to this function.
Solvency
Insurers need capital to absorb risk. It is critical that executive management and the Board understand the specifics of how much capital is needed given the risk profile of the insurer. The sensitivities to changes in investment profile, changes in receivables and changes in reserves should be communicated through internal management training sessions that include the Actuary. Ideally a Board training session should follow where the options for remediation of non-compliance are fully discussed.
The effect on solvency of poor medical performance, medical unexpired risk reserves and overdue medical receivables and payables should be understood and fed into KPIs. Underwriters and management must be aware of limits on the extent to which solvency relief is provided through the use of reinsurance. Major reinsurance decisions should not be taken before assessing the impact on solvency.
Data Analytics
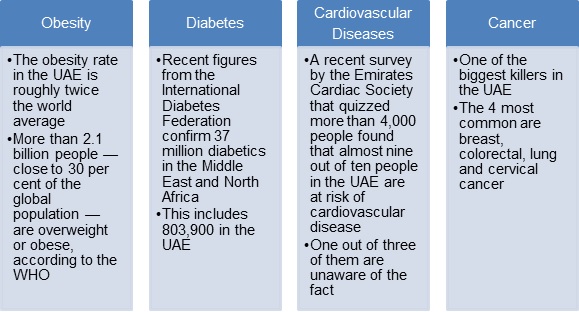
Source: http://gulfnews.com/gn-focus/special-reports/health/the-state-of-the-uae-s-health-2016-1.1658937
With specific reference to medical insurance there is a wealth of information available within medical claims utilisation data sets that can and must speak to the underwriting and claims management functions. International best practice mandates that this data is mined in order to derive insights to reinforce the insurers competitive advantage. The importance of doing so is underscored by the prevailing medical pathology of the resident population. The alarming trend of chronic and pre-existing disease prevalence should concern insurers looking to maintain or grow their medical portfolios. It is important that insurers monitor, at a high degree of detail, the following:
- Analyses of ICD codes in order to understand disease prevalence. The most prevalent codes by volume of treatments usually include the following:
- Acute upper respiratory infection
- Diabetes with and without complications
- Hypertension
- Lower back pain
- Gastritis and gastroenteritis
- Hyperlipidaemia
It’s important that experience on these types of claims are isolated and examined across providers as this experience has a key impact on overall inflation.
- Analyses of providers and specific high cost physicians in order to inform network selections. This is important given the perceived fraud, waste and abuse component of overall medical inflation. Network negotiation is always strengthened with the presence of objective analytics outputs.
- Chronic Disease Management – insurers should identify their chronic patients and implement some form of chronic disease management, particularly for those above 45 years of age. In developed markets predictive modelling is commonplace as insurers look to, amongst other things, isolate high risk groups so as to introduce tailor made response programs that target better patient outcomes.
- Exposed risks – particularly important for portfolios where volumes are increasing is the need to assess claims efficiency standards e.g. fluctuations in rejection ratios. When claims management standards deteriorate this sometimes leads to provider resubmission of claims eventually being paid over 1 year after treatment dates. Reserving, pricing and performance are all compromised if this is not monitored carefully.
- Analysis of large claims and large claim volumes by member – this can be linked to the analysis of chronic patients, for whom the likelihood of large total annual expenses is high, however neoplasms and associated cancer treatments are the usual cases. Screenings do have a role to play here but the effect is seen over a period more than a 1-year horizon. Insurers in developed markets offer critical illness lump sum coverage as a value-added benefit either bundled within medical insurance or provided separately. This can be seen as a useful differentiating feature.
- Claims audits – analytics is a cornerstone of any claims audit department that focuses on identifying instances of fraud, waste and abuse (FWA). Basic dashboards that flag anomalies can be very effective if built with the support of those with medical backgrounds.
- Understand the impact of drug formularies – medication costs are a significant component of overall outpatient costs. Understanding tariff differences of generic versus brand drugs in order to decrease costs without compromising treatment is a critical part of managing inflation.
Board Buy-in
Finally, the culture of the insurer must be consistent with this longer-term focus of medical insurance. Its success rests on being endorsed by the Board and a commitment to allowing the time for this technical focus to bear fruit and drive medical insurance growth. Management must have the buy-in of the Board over the long term if this rehabilitation strategy.
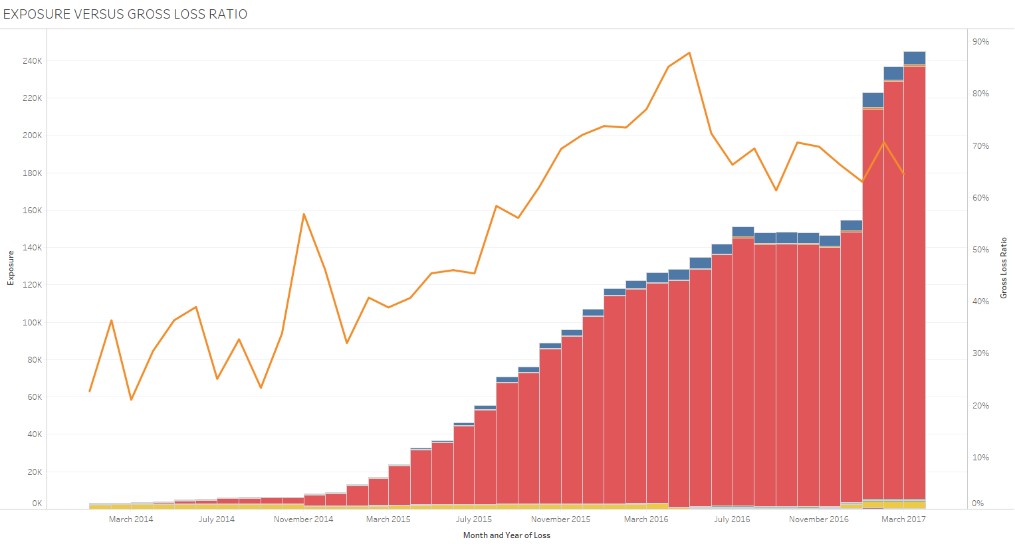
The orange line describes the gross loss ratio whilst the bars denote membership by network. Analysis of changes in loss ratios against increases in exposed lives speak to, amongst other things, claims efficiency.
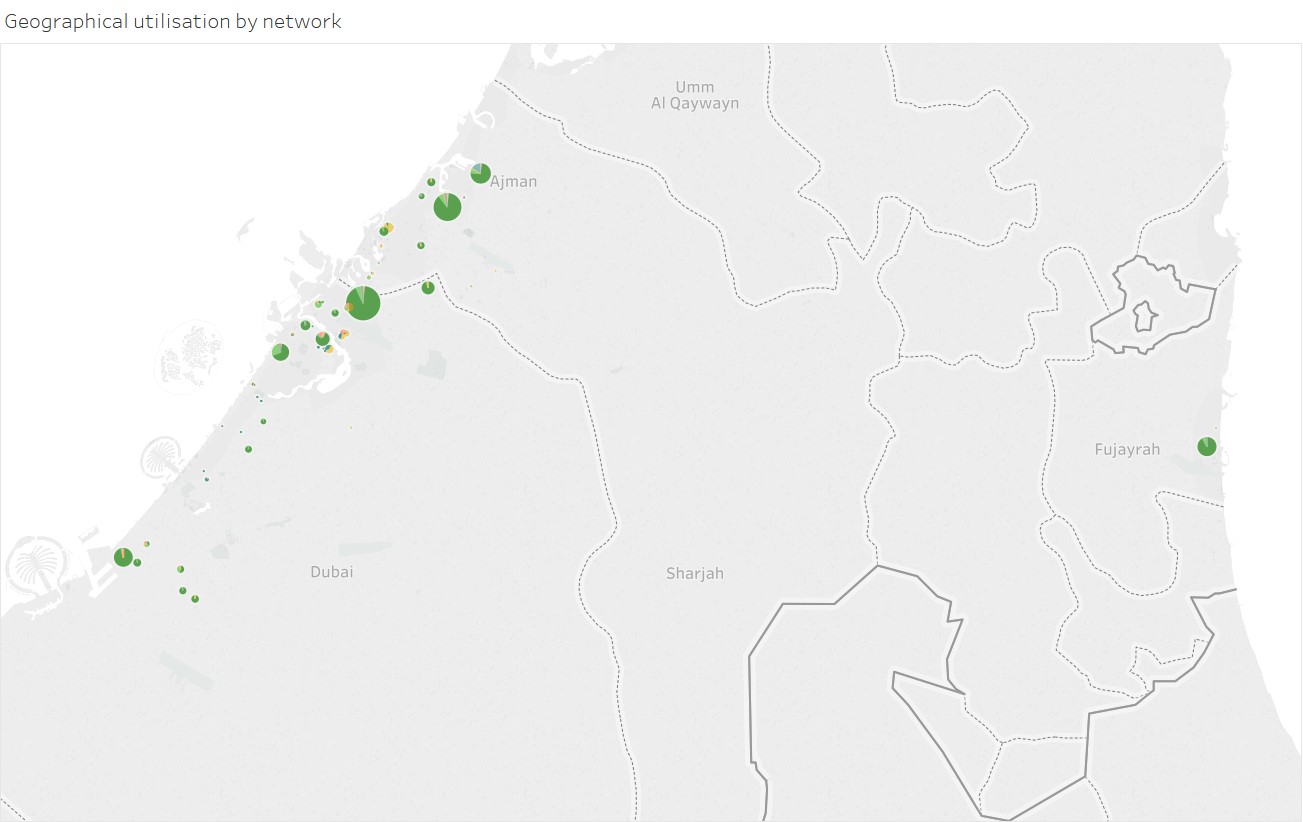
The chart above shows utilisation patterns by provider where each colour denotes a different network and the size of the bubble indicates the relative volume of claims serviced by provider. This illustration helps us to understand utilisation of members outside of their network.
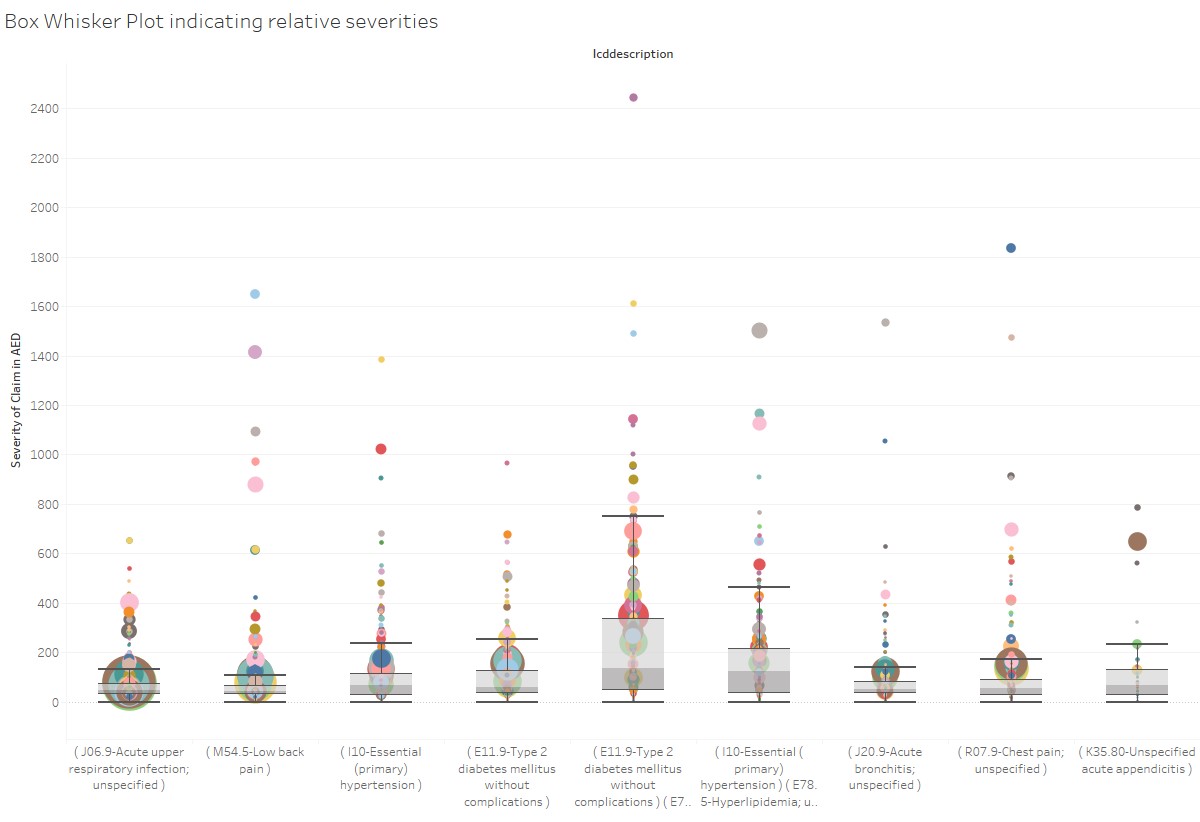
The chart above shows the relative differences of severities for the most common ICDs for a particular claims data set. The size of each bubble denotes the relative volume of claims serviced by a particular provider whilst the colour of each bubble denotes a unique provider. This illustration helps us identify consistently high cost providers with high utilisation.


